Gametogenesis-Oogenesis-Spermatogenesis
Table of Contents
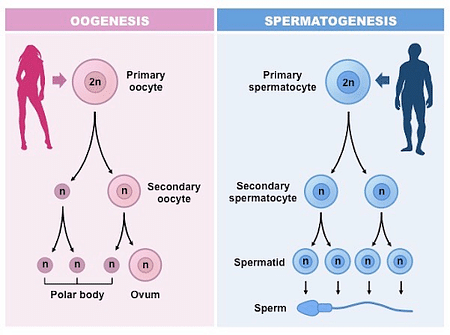
Gametogenesis is defined as the process through which gametes are formed in reproducing organisms. In mammals, the gametogenesis process in males is called spermatogenesis (formation of sperms) and in females, it is called oogenesis (formation of ovum).
Gametogenesis can be of two types –
- Spermatogenesis – formation of sperm in the testes of males.
- Oogenesis – Formation of ovum in the ovary of females.
Gametogenesis
Oogenesis
We have already discussed that oogenesis is the process of formation of ovum within the ovaries. Did you know that in mammals, oogenesis begins even before a female is born? Oogenesis begins in the ovary of a developing female foetus as early as the 25th week of pregnancy. Let us now get into the details of the process.
Oogenesis is completed in three stages – multiplication stage, growth phase and maturation phase.
Multiplication phase
During foetal development, as the process of oogenesis begins, few cells of the germinal epithelium enlarge and undergo repeated mitotic divisions to form a group of germ cells known as oogonia or egg mother cells. Around two to eight million oogonia are formed in the foetal ovary and no more oogonia is added or formed in the ovary after birth. Each oogonia undergoes repeated mitotic division and forms a group of cells which project into the stroma of the ovary in the form of a cord known as the egg tube of Pfluger. This tube soon takes the form of a round egg nest.
Growth phase
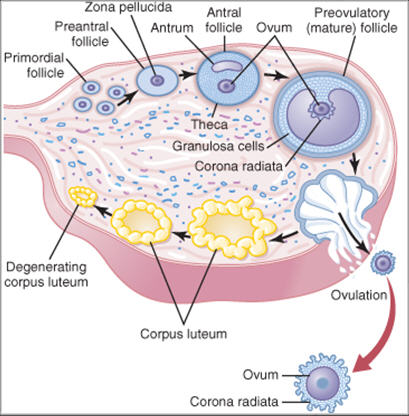
Formation of primary follicle
Only one of the cells within the round egg nest enlarges to become the primary oocyte. The rest of the cells, known as granulosa cells, form a layer around the primary oocyte which is known as the follicular epithelium. The primary oocyte surrounded by the follicular epithelium forms the primary follicle.
The growth phase of the primary oocyte is very long and elaborate and involves a number of changes. The oocyte increases in size many-fold due to accumulation of reserve food materials. The number of mitochondria increases along with the activity of the endoplasmic reticulum and Golgi complex. A vitelline membrane forms around the oocyte. The nucleus of the oocyte increases in size due to increase in nucleic acid content and the number of nucleoli. rRNA genes amplify to synthesise more rRNA which would eventually help in synthesising more ribosomes for protein synthesis.
Maturation phase
The maturation phase begins when the nucleus of the primary follicle starts dividing meiotically but is arrested at the diplotene stage of prophase I at the foetal stage. Further nuclear division occurs only at the age of puberty.
A human female is born with around two million primary oocytes of which many degenerate till she reaches puberty. Only 60,000-80,000 primary follicles remain at the age of puberty, of which only 400-500 mature into ova during a woman’s lifetime.
At puberty, the primary follicles start transforming into secondary follicles and get surrounded by several layers of granulosa cells and a new theca.
The secondary follicle gradually transforms into a tertiary follicle by the appearance of a fluid filled cavity known as the antrum. The fluid is known as the liquor folliculi and provides nutrition to the growing primary oocyte. The formation of the antrum causes the follicular cells of the theca to be organised into an outer theca externa and an inner theca interna.
Formation of Graafian follicle
The tertiary follicle matures into a Graafian follicle. This is the mature mammalian follicle and is about 2.5 cm in diameter. The wall of the Graafian follicle is made up of several layers of granular follicular cells and is divided into theca interna and theca externa. A fluid filled cavity called the antrum is present which is filled with the fluid liquor folliculi secreted by the follicular cells. The oocyte is attached to the granulosa cells of the follicular wall with the help of a cluster of cells known as cumulus oophorus. The secondary oocyte in the Graafian follicle is surrounded by a thick, non-cellular layer known as the zona pellucida and a layer of follicular cells known as the corona radiata.
Completion of first meiotic division and formation of secondary oocyte
Within the Graafian follicle the primary oocyte grows in size and it completes the first meiotic division which leads to the formation of a haploid secondary oocyte and a haploid polar body. The division of ooplasm (cytoplasm of the oocyte) is unequal and the secondary oocyte retains most of the nutrient rich cytoplasm of the primary oocyte while the first polar body receives very less ooplasm. As for the fate of the first polar body, nothing is known. It is known to have no function.
The nucleus of the secondary oocyte enters into the second meiotic division. At the time of ovulation, the mature graafian follicle rises to the surface of the ovary and ruptures to release the egg or ovum at the secondary oocyte stage with its nucleus arrested at the metaphase II stage of the second meiotic division. This process is known as ovulation.
The secondary oocyte completes the second meiotic division only after it is fertilised by a sperm. The completion of the second meiotic division also results in the formation of an ovum and a second polar body. Meanwhile, the first polar body also completes the second meiotic division and forms two polar bodies. Thus, after the completion of meiosis of the primary oocyte, a haploid ovum and three haploid polar bodies are formed. The polar bodies have no function. If the fertilisation does not occur within 24 hours of ovulation, the oocyte degenerates remaining arrested in meiosis II of cell division.
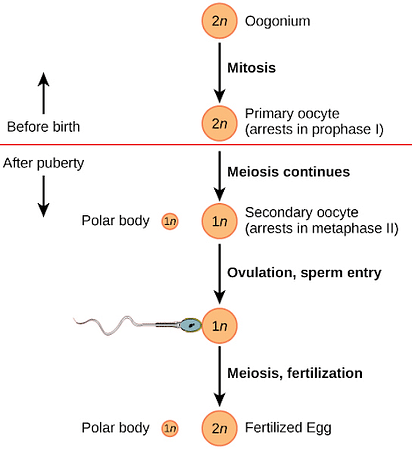
Fig: Meiotic division during oogenesis
The ruptured Graafian follicle is left containing a blood clot known as the corpus haemorrhagic. The follicular cells of the ruptured follicle form a yellowish mass which is known as the corpus luteum. It is responsible for the secretion of the progesterone and relaxin hormones. In the absence of fertilisation, the corpus degenerates in about a week and appears as a white mass known as corpus albicans.
Ovulation
The mature Graafian follicle reaches the surface of the ovary and ruptures to release the secondary oocyte by the process of ovulation. It is caused by the increased turgidity in the follicle. Contraction of the smooth muscles around the follicle also helps in the process. In human females, only one egg is released from either one of the ovaries during ovulation of a menstrual cycle.
Hormones – Oogenesis
The hypothalamus releases the gonadotropin releasing hormone (GnRH) which stimulates the anterior pituitary to release two gonadotropic hormones named FSH (follicle stimulating hormone) and LH (Luteinising hormone). FSH stimulates follicular growth and oocyte maturation. The granulosa cells of the developing follicles also release a hormone named oestrogen. When the level of oestrogen and LH becomes very high, the Graafian follicle ruptures and releases the egg by the process of ovulation. High concentration of oestrogen prevents further release of GnRH and FSH.
LH promotes the conversion of the ruptured Graafian follicle into corpus luteum which secretes progesterone. Progesterone promotes development of the uterus to prepare itself for receiving the fertilised zygote.
In case of fertilisation, the corpus luteum persists and as progesterone levels increase, it inhibits further secretion of GnRH and consequently the release of FSH, LH and oestrogen is also inhibited. This prevents further growth and maturation of follicles and hence no ovulation occurs as long as pregnancy is maintained.
In case there is no fertilisation, the corpus luteum degenerates and the uterine lining sheds. As the level of progesterone goes down, the release of GnRH increases and the body gets ready for the next menstrual cycle and development of primary follicles.
The role of hormones in oogenesis is to regulate the development and maturation of the female gametes, or eggs, in the ovaries. Hormones are chemical messengers that are produced by endocrine glands and travel through the bloodstream to target organs. The main hormones involved in oogenesis are:
- Gonadotropin-releasing hormone (GnRH): This hormone is released by the hypothalamus, a part of the brain that controls many bodily functions. GnRH stimulates the anterior pituitary gland, another endocrine gland in the brain, to secrete two other hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- Follicle-stimulating hormone (FSH): This hormone stimulates the growth and development of the ovarian follicles, which are structures that contain the primary oocytes, or immature eggs. FSH also induces the production of estrogen by the follicular cells, which are the cells that surround the oocytes.
- Estrogen: This hormone is produced by the follicular cells and has several functions in oogenesis. Estrogen promotes the growth and maturation of the oocytes and the follicles, prepares the uterus for implantation of a fertilized egg, and inhibits the secretion of FSH by the anterior pituitary gland through a negative feedback mechanism. Estrogen also triggers a positive feedback mechanism that causes a surge of LH secretion by the anterior pituitary gland.
- Luteinizing hormone (LH): This hormone is responsible for inducing ovulation, which is the release of a secondary oocyte, or mature egg, from the ovary. LH also stimulates the transformation of the ruptured follicle into a structure called the corpus luteum, which produces another hormone: progesterone.
- Progesterone: This hormone is produced by the corpus luteum and has several functions in oogenesis. Progesterone maintains the thickness and blood supply of the uterine lining, supports the implantation and development of a fertilized egg, and inhibits the secretion of GnRH, FSH, and LH by the hypothalamus and the anterior pituitary gland through a negative feedback mechanism. If the egg is not fertilized, the corpus luteum degenerates and the levels of progesterone drop, leading to the shedding of the uterine lining, or menstruation.
These hormones work together to coordinate the process of oogenesis and the menstrual cycle, which are the main events of female reproduction.
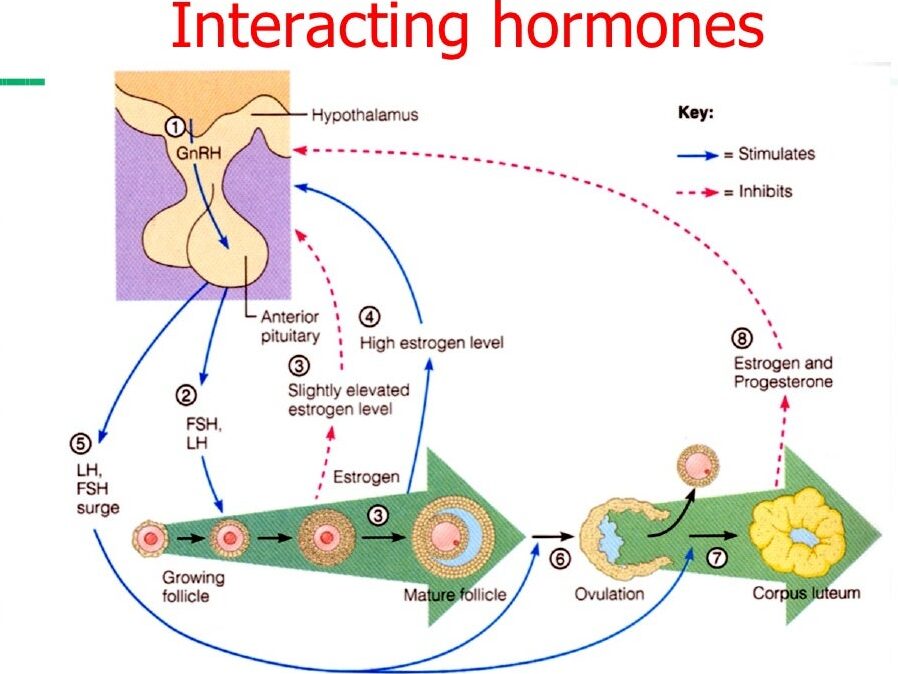
Fig: Hormonal control of oogenesis
Spermatogenesis vs Oogenesis
Similarities
- Both the processes occur in the germ cells of the gonads.
- Both result in the formation of haploid gametes
- Both the processes involve a multiplication phase, a growth phase and maturation phase.
- In both the processes, changes occur in both the nucleus and the cytoplasm of the primary spermatocyte and primary oocyte.
Differences
- Spermatogenesis begins at puberty in males whereas the process of development of oocytes for oogenesis begins at the foetal stage during the 25th week of development.
- Spermatogenesis results in the formation of millions of sperm cells (male gametes) but oogenesis results in the formation of only one egg or ovum (female gamete) during each menstrual cycle.
- In spermatogenesis, the spermatogonia go through four more stages to form the sperm, namely, primary spermatocyte, secondary oocyte, spermatids and spermatozoa or sperm. In oogenesis, the oogonia go through three stages only, primary oocyte, secondary oocyte and finally form the ovum.
- During spermatogenesis, meiosis results in equal cell division and formation of four spermatids. During oogenesis, the meiotic divisions are unequal and result in the formation of a single large ovum and three small non-functional polar bodies.
Ploidy
Ploidy level of Nucellus, Endosperm, Polar nuclei, Megaspore mother cell, female gametophyte respectively are
- Nucellus, microspore mother cells (MMC), and megaspore mother cells are part of sporophyte so these are diploid cells and their ploidy is 2n. And female gametophytes are part of gametophyte and ploidy is n.
- The endosperm constitutes an organism separate from the growing embryo. About 70% of angiosperm species have polyploid endosperm cells. These are typically triploid but can vary widely from diploid (2n) to 15n.
- Sperm released fuses with the two polar nuclei forming a triploid cell that develops into the endosperm.
- A megaspore mother cell is a diploid cell in which meiosis occurs, resulting in the production of four haploid megaspores.
- Hence, Ploidy level of Nucellus, endosperm, polar nuclei, Megaspore mother cell, female gametophyte respectively are 2n,3n,n,2n,n.
Q1. At which stage of the cell cycle are primary oocytes arrested till they reach puberty?
a) Diplotene stage of Prophase I
b) Diakinesis stage of Prophase I
c) Leptotene stage of Prophase I
d) Zygotene stage of Prophase I
ANSWER
Oogonia or the egg mother cells are formed during the 25th week of foetal development. The oogonial cells divide mitotically and multiply to form a round egg nest. Only one of the oogonial cells enlarges and becomes the primary oocyte while the rest of the follicular cells surround it and together they form the primary follicle. During the maturation phase, the primary oocyte enters the first meiotic division but it gets arrested at the diplotene stage of prophase I until the individual reaches puberty. Hence the correct option is (a). Diplotene stage of Prophase I
Q2. A female born with two million primary oocytes in each ovary can produce a maximum of more than two million eggs in her lifetime. Is the given statement true or false?
ANSWER
Oogenesis begins during the 25th week of foetal development and from the diploid oogonial cells, around two million primary oocytes are formed which remain arrested at the diplotene stage of prophase I of their first meiotic cell division, until the reach puberty. No more primary oocytes are formed or produced after birth. By the time a female reaches puberty, many oocytes degenerate and only around 60,000-80,000 oocytes remain. Of these, only around 400-500 eggs are able to mature in a woman’s lifetime. Even if there was no degeneration of oocytes, the maximum number of eggs would not have exceeded two million as no new oocytes are formed after birth. Thus, the given statement is false.
Q3. Choose the option which shows the correct ploidy for the given cell types
a) Primary oocyte: 2n; Secondary oocyte: n; Ovum: n
b) Primary oocyte: n; Secondary oocyte: 2n; Ovum: n
c) Oogonium: 2n; Primary oocyte: n; Secondary oocyte: 2n
d) Oogonium: n; Primary oocyte: 2n; Secondary oocyte: 2n
ANSWER
This is because the primary oocyte is formed by the first round of meiosis from the diploid oogonium, and it is arrested at prophase I until ovulation. Therefore, it has the same number of chromosomes as the oogonium, but twice the amount of DNA. The secondary oocyte is formed by the completion of meiosis I, and it receives most of the cytoplasm and half of the chromosomes from the primary oocyte. The other half of the chromosomes forms a polar body, which is discarded. The secondary oocyte is arrested at metaphase II until fertilization. The ovum is formed by the completion of meiosis II, and it receives all of the chromosomes from the secondary oocyte. The other set of chromosomes forms another polar body, which is also discarded. The ovum is the mature egg cell that can be fertilized by a sperm cell
Hence the correct option is (a). Primary oocyte: 2n; Secondary oocyte: n; Ovum: n
Q4. A person with 4n chromosomes will have _______ set of chromosomes in their first polar body.
a) n
b) 3n
c) 2n
d) more than 4n
ANSWER
During oogenesis, meiotic division occurs and results in halving the number of chromosomes in the daughter cells. The oogonial cells of a person will have the same number of chromosomes as his somatic cells. Thus, a person with 4n number of chromosomes will have 4n ploidy in the oogonial cells too. One of the oogonial cells grows into the primary oocyte which will also have 4n chromosomes. As the primary oocyte completes the first meiotic division, it results in the formation of a secondary oocyte and a first polar body, each of which will have half the number of chromosomes compared to the primary oocyte. Thus, the first polar body will have 2n number of chromosomes.
Hence the correct option is (c).2n
Q5. How big is an egg cell compared to a sperm?
ANSWER
In humans, the egg cell is around 10,000 times larger than the sperm cell.
Q6. Why are egg cells larger than sperm cells?
ANSWER
Egg cells need to store a lot of food for the growing embryo after fertilisation and also need a large number of mitochondria to produce enough energy to power the growth. Thus, they grow very large in size. Sperms on the other hand are small in size in order to increase the chances of fertilising the ovum. Production of a large number of sperms is possible owing to the tiny size of sperms.
Q7. What does ‘freezing one’s eggs’ mean?
ANSWER
Freezing the eggs is a technique of cryopreservation of oocytes. The oocytes are extracted, frozen and stored to be used in future. This helps to preserve the reproductive potential of women who are at a reproductive age but are not in a position or mindset to give birth. When the woman is ready, the eggs are thawed in a warming solution and the viable eggs are directly injected with sperm with the intracytoplasmic sperm injection (ICSI) technique. Once the egg is fertilised, within 3-5 days the embryos become ready and can be transferred to the uterus to achieve pregnancy. The chances of success are about 4-12% per oocyte.
Q8. What triggers the completion of the second meiotic division in the secondary oocyte?
ANSWER
At the time of ovulation, the egg is released at the secondary oocyte stage and its nucleus is arrested at the metaphase II stage of meiosis. As the sperms enter the egg cell by penetrating the zona pellucida they bring about certain changes in the cytoplasm of the egg. The ER releases lots of Ca2+ ions into the cytoplasm which induce activation of the anaphase promoting complex (APC) and the metaphase promoting factor (MPF) is removed. This triggers the secondary oocyte to move forward to the metaphase II stage and complete the second meiotic division.
Q9. (NEET 2022 question)Which of the following statements are true for spermatogenesis but do not hold true for Oogenesis ?
(a) It results in the formation of haploid gametes
(b) Differentiation of gamete occurs after the completion of meiosis
(c) Meiosis occurs continuously in a mitotically dividing stem cell population
(d) It is controlled by the Luteinising hormone (LH) and Follicle Stimulating Hormone (FSH) secreted by the anterior pituitary
(e) It is initiated at puberty
Choose the most appropriate answer from the option give below :
- (b), (c), and (e) only
- (c) and (e) only
- (b) and (c) only
- (b), (d) and (e) only
ANSWER
Q10. (NEET 2022 question) At which state of life the oogenesis process is initiated?
- Adult
- Puberty
- Embryonic development stage
- Birth
ANSWER
Embryonic development stage
Take Quiz
1. A/An ________ is released at the time of ovulation.
(a) oogonium
(b) primary oocyte
(c) ovum
(d) secondary oocyte
ANSWER
d) secondary oocyte
2. Rapid secretion of _____ induces ovulation.
(a) FSH
(b) estrogen
(c) progesterone
(d) LH
ANSWER
d) LH
3. One primary oocyte produces _ female gamete(s).
(a) 4
(b) 2
(c) 3
(d) 1
ANSWER
d) 1
4. Which of the following hormones stimulates the development of ovarian follicles?
(a) FSH
(b) estrogen
(c) progesterone
(d) LH
ANSWER
a) FSH
5. The process of formation of a mature female gamete is called ________.
(a) spermatogenesis
(b) menstruation
(c) ovulation
(d) oogenesis
ANSWER
d) oogenesis
6. The non-cellular membrane of human ovum is called ________.
(a) zona pellucida
(b) zona radiata
(c) membrana granulosa
(d) vitelline membrane
ANSWER
a) zona pellucida
7. The division in primary oocytes arrests at _______ stage.
(a) prophase of meiosis I
(b) metaphase of meiosis I
(c) prophase of meiosis II
(d) metaphase of meiosis II
ANSWER
a) prophase of meiosis I
8. The division in secondary oocytes arrests at _______ stage.
(a) prophase of meiosis I
(b) metaphase of meiosis I
(c) prophase of meiosis II
(d) metaphase of meiosis II
ANSWER
d) metaphase of meiosis II
9. Capacitation is the change in ________.
(a) sperm after fertilisation
(b) ovum after fertilisation
(c) ovum before fertilisation
(d) sperm before fertilisation
ANSWER
d) sperm before fertilisation
10. Meiosis II in secondary oocytes is not completed until ________.
(a) birth
(b) uterine implantation
(c) fertilisation
(d) puberty
ANSWER
c) fertilisation
